There is a common reproductive disease which 1 in 20 women will develop in their lifetime. It can cause chronic abdominal pain, difficulty getting pregnant, ectopic pregnancy, and infertility.[1] There is no test for it; in fact, it can only be diagnosed by a nurse or doctor. Have you heard of pelvic inflammatory disease?
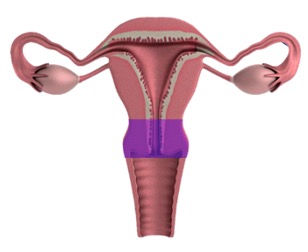
Pelvic Inflammatory Disease (PID) is an infection of the female upper reproductive tract – the uterus, fallopian tubes, and ovaries (highlighted in purple below).
What causes PID?
PID occurs when bacteria in the lower reproductive tract – the vagina – spread upwards into the uterus. The most common infections known to cause PID are chlamydia, gonorrhea, and bacterial vaginosis. Even some respiratory bugs have been associated with PID. [2]
STDs (the most common)
Common STDs, such as gonorrhea and chlamydia, can cause infection with few or no symptoms. As a result, the infection can worsen and spread without the person ever knowing. PID can occur when these bacteria migrate from the vagina into the uterus.
Bacterial Vaginosis
Generally, the vagina is populated with lots of good bacteria. These bacteria keep the vaginal environment acidic – about as acidic as a glass of wine – which keeps other disease-causing bacteria, viruses, fungi, and parasites at bay. The good bacteria exist in important proportions relative to one another. An infection called bacterial vaginosis results when these proportions are thrown off. PID can result when the bacterial-vaginosis-causing pathogens travel into and infect the uterus.
Typical Vaginal Bacteria
As discussed earlier, the vagina has its own microbiome of safe, healthy bacteria. While the presence of bacteria in the uterus is still being researched, the uterus is generally more sterile than the vagina. The cervix (highlighted in purple below) is a narrow channel covered with mucus that keeps the vagina and body of the uterus separate. However, sometimes bacteria from the vagina make their way through the cervix, into the uterus, and cause infection. For this reason, women and girls who have never had sex can still develop PID (although this is generally rare). [3]
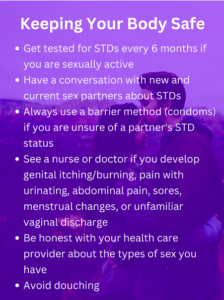
In any of the three causes outlined above, pathogens needed to travel from the vagina and into the uterus. Although this can happen spontaneously (for reasons that are still being understood), certain practices can make this more probable, including sex with a penis and douching.
1) Sex with a penis. During sexual arousal, the cervix naturally changes shape to allow sperm to enter the uterus. This makes it more possible for fluids, both vaginal fluids and semen, to enter the uterus. If you or your partner has an STD, this can allow the bacteria into the uterus, which puts you at higher risk of developing PID. [4]
2) Douching. Using water or soaps to clean the vagina can wash away good bacteria, which advantages infection-causing bacteria. As a result, you are at higher risk of contracting STDs and/or developing bacterial vaginosis, which increases the likelihood of developing PID.
Douching is a particularly dangerous practice that is not required or necessary. Unfortunately, there is a false belief that vaginal douching is required to be personally hygienic or sexually appealing to others. [5] Forget this! Douching disrupts the vagina’s natural microbiome and can make odor-causing infections, like bacterial vaginosis and yeast, more likely. The reality is that every healthy vagina and vulva will have a characteristic smell, and that’s just fine. As long as you are practicing good hygiene (washing your external genitals regularly, wiping correctly) and keeping yourself protected from infections, there’s no need to worry about your normal smell.
PID is COMMON
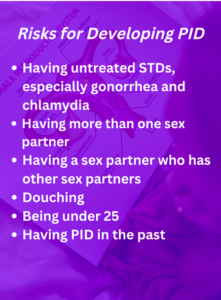 Although about 4% of women will develop PID, it is much more common in younger women and girls. In fact, about 12.5% of women under age 19 will develop PID, compared to 1.3% of women over age 24. This is thought to be because of (1) higher rates of STDs in young people and (2) young people tend to engage in risky sex more often. [6]
Although about 4% of women will develop PID, it is much more common in younger women and girls. In fact, about 12.5% of women under age 19 will develop PID, compared to 1.3% of women over age 24. This is thought to be because of (1) higher rates of STDs in young people and (2) young people tend to engage in risky sex more often. [6]
In addition, the anatomy of an adolescent female’s reproductive system may make them more susceptible to PID. The maturing cervix tends to have a higher proportion of tissue that is susceptible to infection – called glandular epithelium – than the matured cervix. In addition, as an adolescent female body becomes accustomed to menstruation, the cervical mucus (which protects the uterus from infection) is often thinner and more watery than an adult woman, making it easier for pathogens to infect. These two anatomical and hormonal differences put adolescent girls at higher risk of developing PID. [7]
PID is SERIOUS
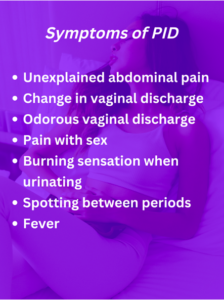
Although PID is common, it is an incredibly serious infection. Early identification and treatment are critical to prevent long-term side effects from the infection. 25% of women who develop PID will experience a serious complication, including recurrent PID, chronic pelvic pain, ectopic pregnancy, and infertility. Delaying treatment by as little as three days has been shown to significantly increase the risk for these complications. [8]
PID is TREATABLE
 Unlike STDs and bacterial vaginosis, there is no “test” that identifies PID. A doctor or nurse will use clinical clues, like your reported symptoms, sexual history, STD results, or an ultrasound of your uterus/ovaries, to decide whether PID is likely present or not. Because PID is so serious, doctors are trained to generally treat women for PID if there is a concern for it, even if they are not 100% certain that it is present.
Unlike STDs and bacterial vaginosis, there is no “test” that identifies PID. A doctor or nurse will use clinical clues, like your reported symptoms, sexual history, STD results, or an ultrasound of your uterus/ovaries, to decide whether PID is likely present or not. Because PID is so serious, doctors are trained to generally treat women for PID if there is a concern for it, even if they are not 100% certain that it is present.
Generally, if a woman or girl is deemed at risk for STIs (is sexually active or has experienced sexual assault) and has pelvic or lower abdominal pain with no other identified cause (such as food poisoning or a urinary tract infection), doctors will treat PID presumptively.
The only way PID can be treated and cured is through antibiotics given orally, intramuscularly, or through an IV for up to 14 days. This antibiotic cocktail – generally Ceftriaxone, Doxycycline, and Metronidazole – covers a large spread of pathogens that may be responsible for the infection. Although it is vitally important to finish the 14-day course of antibiotics, many women start feeling markedly better in just a few days. [9]
[1] CDC “Pelvic Inflammatory Disease”
[2] Curry A, Williams T, Penny ML. Pelvic Inflammatory Disease: Diagnosis, Management, and Prevention. Am Fam Physician. 2019 Sep 15;100(6):357-364. PMID: 31524362.
[3]Algren SD, Strickland JL. Beta Hemolytic Streptococcus Group F Causing Pelvic Inflammatory Disease in a 14-Year-Old Girl. Journal of Pediatric and Adolescent Gynecology. 2005;18(2):117-119. doi:10.1016/j.jpag.2005.01.007
[4] Planned Parenthood, “Cervical Health 101”
[5] Martino JL, Vermund SH. Vaginal douching: evidence for risks or benefits to women’s health. Epidemiol Rev. 2002;24(2):109-124. doi:10.1093/epirev/mxf004
[6] Gray-Swain MR, Peipert JF. Pelvic inflammatory disease in adolescents. Current Opinion in Obstetrics & Gynecology. 2006;18(5):503-510. doi:10.1097/01.gco.0000242952.87125.69
[7] Gray-Swain, et al
[8] Gray-Swain, et al
[9] CDC “Pelvic Inflammatory Disease (PID) – STI Treatment Guidelines”
 Emma Hergenrother is from Ridgefield, CT. She is excited to be currently living in Durham, NC, and contributing to Women AdvaNCe as a Research Fellow. Earning her Bachelor’s from Princeton University, Emma majored in religion with a focus on the relationship between religious attitudes, theological beliefs, and environmentalism. Since graduation, Emma has worked for an affordable housing nonprofit in Connecticut, and is currently studying to become a physician with a focus on pediatric health. In her free time, Emma enjoys cooking with her partner, going for long walks, and diving into her latest audiobook.
Emma Hergenrother is from Ridgefield, CT. She is excited to be currently living in Durham, NC, and contributing to Women AdvaNCe as a Research Fellow. Earning her Bachelor’s from Princeton University, Emma majored in religion with a focus on the relationship between religious attitudes, theological beliefs, and environmentalism. Since graduation, Emma has worked for an affordable housing nonprofit in Connecticut, and is currently studying to become a physician with a focus on pediatric health. In her free time, Emma enjoys cooking with her partner, going for long walks, and diving into her latest audiobook.


There are no comments
Add yours